Applying the Kelley Model for Community Capacity Development
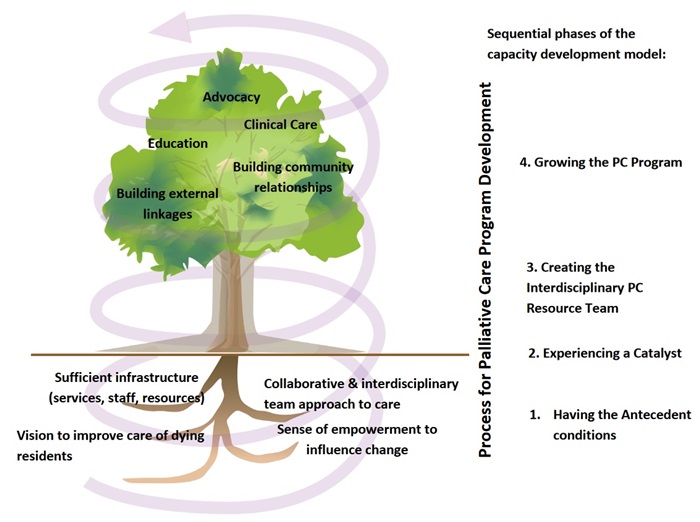
A community capacity development model developed by Dr. Mary Lou Kelley was adapted for use as a theory of change to develop the Palliative Care programs in the long term care (LTC) homes. The original model was developed, evaluated and validated in rural communities. However, the inherent values and theory of community capacity building translate well into any community setting including LTC homes. The four phase model, depicted in figure 1 below as a growing tree, illustrates a bottom-up & sequential change process.
The model for developing palliative care programs occurs in four phases. The phases outline a dynamic, sequential, but gradual transformative process in organizational culture and care processes over time. Each phase includes a number of activities or processes that grow out of and build upon those of the previous phase; however, work in all phases is ongoing. Progression through the phases is influenced by barriers, supports and resources that are both internal or external to the LTC home and the palliative care program. Keys to success are identified for each phase.
When the program has evolved into phase four, palliative care program capacities include: provision of clinical palliative care to residents; palliative care education; advocacy; creation of community relationships to improve continuity of care; and building external linkages with regional palliative care experts for education and consultation.
The model is visually depicted below.
Each phase of the model is elaborated below:
Phase 1: Antecedent Conditions in the LTC Home
In the model, four antecedent conditions must all be in place prior to beginning program development. These antecedent conditions determine readiness and together they form the foundation for palliative care development. These conditions must preexist if development is to be successful. Where significant gaps exist, addressing these before proceeding is required. The four conditions are:
- having sufficient health care infrastructure (interdisciplinary staff, services, education, resources/equipment, facilitative organization policies and clinical protocols)
- having a collaborative and interdisciplinary team approach to care
- having a shared vision to improve care of dying residents and to support them to die at home in long term care
- having a sense of control/empowerment within the LTC home to make changes in the organization
Project Outcomes:
LTC homes can assess their antecedent conditions through staff/management discussions and use of tools such as the QPC-LTC Self-Assessment Tool that is found in the Tool kit under organizational change. Keys to successful development in this first preparatory phase include staff and managers working together, and being resident-focused.
In our research, the environmental assessment identified the following barriers in the LTC homes: staff lacked knowledge of PC and access to PC education; there was no comprehensive resident Palliative Care assessment and no systematic process to identify residents approaching end-of-life; the LTC home lacked policies and procedures relating to PC; communication problems existed amongst staff, residents, and families regarding PC issues.
Phase 2: Experiencing a Catalyst for Change
A catalyst for change occurs for staff in the LTC home, disrupting their current practice, creating strong motivation and initiating change in their approach to caring for dying people. This catalyst can be internal such as a person (e.g a palliative care champion amongst the staff) or an event such as a "bad death". It can initiate externally, for example, a new palliative care policy or funding, or staff participating in palliative care education. However, while the change can be initiated outside of the LTC home, to be a true catalyst the momentum for change must be internal.
Project Outcomes
In our research, we engaged highly motivated, passionate and committed personal support workers within each home who were champions for change, and a senior manager in each home to sponsor their work. The front line staff were the catalyst to create change within the four participating LTC homes. The change process was facilitated by the Alliance researchers and reinforced by enactment of new LTC home legislation in the province that required palliative care education for staff.
Phase 3: Creating a Palliative Care Resource Team
The internal champions motivate other LTC staff to form a palliative care resource team so that they could work together collectively to improve care of their dying residents and develop a palliative care program. This team includes representatives of all the disciplines working in the home, especially the personal support workers who provide the front line care. This is a leadership team and not a clinical team since all LTC staff are involved in providing care to residents. Having solid management support and an identified manager as a sponsor for the palliative care team is important. Other important roles are PSW Champion(s) and a staff member to act as team facilitator. The LTC physician may or may not attend team meetings, but the physician needs to be engaged, informed and supportive of the work. Major themes in creating the team include:
- having dedicated people as team members and
- getting the right people involved (front line staff, registered staff, managers, physicians) Keys to success in this phase include: working together (strong relationships, communication, support), dedication of the team members, and physician involvement.
Project Outcomes
An interdisciplinary Palliative Care Resource Team was developed using a full day planning retreat and a series of meetings to engage the staff. The focus was on engaging direct care workers. A resource for conducting the retreat organizing a process mapping to identify current practices and required changes in palliative care can be found in the toolkit under the organizational change section. Educational modules on the palliative approach, use of the PPS and other relevant topics can be found in the toolkit under education.
Phase 4: Growing the Palliative Care Program
The palliative care resource team continues to build, and is now ready to deliver palliative care. Major themes include:
- strengthening the team,
- engaging the LTC staff of all disciplines/roles
- engaging community PC experts and resources to support the staff
- sustaining the palliative care program
The team is strengthened through education, members sharing their knowledge and skills amongst themselves, and by creating linkages with experts outside the LTC home. Team members build their confidence for providing palliative care. Teams now begin to implement new clinical practices, educate and support their colleagues and peers, and reach out to build community relationships to improve service delivery. Team efforts evolve to include managing challenges, getting additional resources and developing policies needed to sustain the new program. The keys to team success for growing the program were: remaining resident-focused; educating LTC staff and community resources; working together/teamwork; having leadership and feeling pride in their accomplishments.
Project Outcomes
The four LTC homes created their own palliative care programs, policies and procedures while engaging staff, residents and families. Through research and a staff-led quality improvement process, over 40 resources, tools and innovations were developed or adapted to support PC program development in a long term care home. A few examples are provided below.
Enhancing Clinical Care
Creating opportunities for staff to improve clinical skills through working in a Simulation Lab; visiting a specialty Hospice Palliative Care Unit, participating in "Comfort Care Rounds" where residents’ care plans were reviewed with a PC consultant.
Enhancing Education
A 6-module (12 hr.) PC education course was offered for direct care workers; a Snoezelen therapy training program was created and staff, family and volunteers were engaged to use the resource; "book chats" focusing on understanding dementia were initiated with front line staff.
Advocating for PC
Based on the research, a brief was presented to the Canadian Federal Parliamentary Committee on Palliative & Compassionate Care to advocate for resources and policy to support the provision of palliative care in long term care homes.
Building External Linkages
Hospice volunteers & divinity students were engaged to work in the LTC homes to support staff in provision of social & spiritual care.
All toolkit resources are available at no cost and downloadable from the project website.